The inflammation of tooth nerves is called dental pulpitis, which can be reversible and irreversible.
An individual tooth comprises three types of tissues: enamel, dentine, and pulp.
The enamel and dentine are the mineralized parts of the tooth, while the pulp consists of the nerves, connective tissues, lymphatic tissues, and blood vessels.
Whenever a tooth decays and the carious lesion that houses bacteria eats up the mineralized portion of the tooth and comes close to the pulp, you may suffer sensitivity or pain.
Not only caries cause pulpitis, but also trauma to a tooth, and an attempt to save a tooth with a dental procedure can lead to pulpitis.
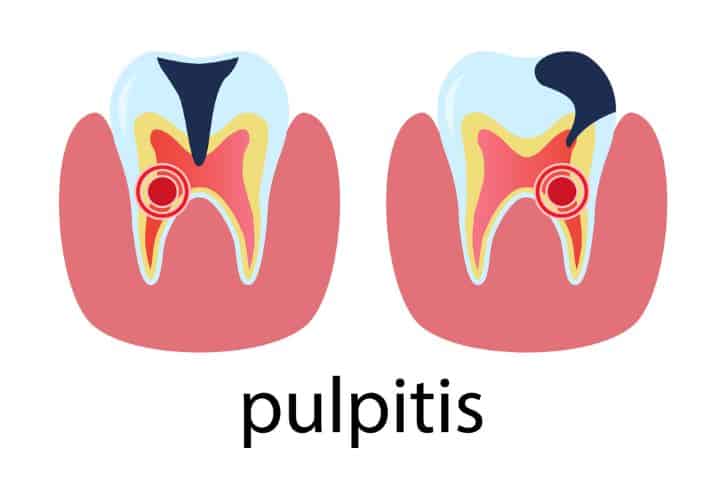
What is Pulpitis?
Pulpitis is made up of two terms: the pulp, which is a dental tissue, and the -itis, which means inflammation.
In simpler terms, inflammation of the tooth nerves is called pulpitis.
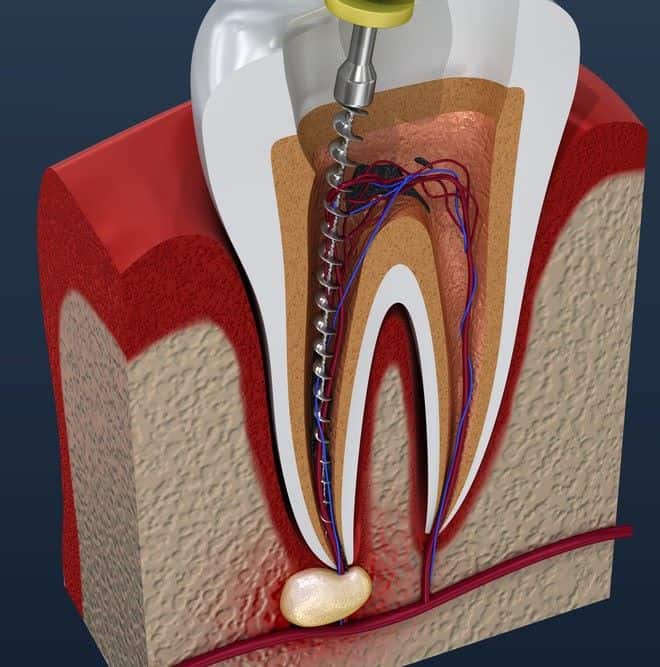
To understand tooth nerve inflammation, let’s take a closer look at the anatomy of the tooth. A tooth is made up of pulp, dentine, and enamel.
The dental pulp comprises nerves, lymphatic vessels, connective tissues, and blood vessels. The dentine is interspersed with the small dentinal tubules directly connected to the pulp.
The enamel is the harder mineralized covering of the tooth. A significant tooth defect like a dental cavity causes a large injury to the dentine.
The greater the dentinal injury, the greater the probability of inflammatory reaction within the pulp.
In general, two mechanisms cause inflammation of the dental pulp:
1 – Infectious Cause:
Such damage occurs when a tooth is carious, and the bacteria that harbor the cavity make their way through dentinal tubules into the pulp.
2 – Non-infectious Cause:
Such damage occurs when a tooth gets physical trauma through a hit, a fall, or chemical damage by dental drilling or chemicals.

The distinction is essential to know the course of the disease. The infectious cause can quickly spread from their pulp into the bone, leading to bone infection if left untreated.
However, the noninfectious cause is equally damaging. The physical trauma to the tooth can lead to pulpal death, which is called pulpal necrosis.
The body has a natural tendency to eliminate all the dead tissues from the body, leading to root canal calcification, also called root sclerosis.
Over time, the root calcifies further and becomes the bone.
- Importance of the dental pulp
Dental pulp keeps the tooth alive or vital. It performs a lot of functions to maintain tooth health, which include:
- Bacterial Protection: The immune cells in the dental pulp can fight the invading bacteria from dentinal tubules to save the vitality of the dental pulp.
- Sensation: The nerves and blood vessels inside the pulp are phenomenal at providing you with information about the temperature and pressure changes on the tooth. This helps you take immediate action against tooth problems to save yourself from high-end solutions like root canal treatment and extractions.
- Dentine Formation: The pulpal tissue has dentine formation cells that form secondary and tertiary dentine over time in response to local injury or trauma to save the pulp.
- Nutrient Circulation: The tooth allows nutrient circulation from within the blood into the tooth. This keeps the dentine healthy and keeps the tooth vital. The pulp also can make proteins like albumin to maintain pulpal health.
Understanding The Outcomes Of Pulpitis
Our immune system can recognize and eliminate structures that are foreign to our body. The marker cells acknowledge and mark the foreign particles, including viruses, bacteria, cell debris, or dead cells.
Afterward, our immune cells eat the foreign materials to subside the infection. The focus of the infection must be surrounded by the blood that has immune cells to eliminate the infection.
The necrotic pulp has no blood supply, which means the bacterial community gets an ideal surrounding to hide from the body’s immune system.

They can feed on the debris and can multiply significantly without any hindrance.
Once the bacterial count improves significantly, the bacteria spread into the bone through the root end, leading to bone infection. It depends on a lot of factors, which include:
- the ability of the immune system
- the immune status of patients
- the number of bacterial counts
- the anatomy of the tooth
- the aggressiveness of the cause
All these factors also define the type of tooth pain you may experience when you suffer from pulpitis. They can be:
- pounding
- pressing
- dull sensation
- excruciating
- non-locatable
It’s essential to take localized infection seriously because bacteria hide at places where immune system access is far lower, like around prosthetic heart valves or dental implants.
At such locations, the bacteria can further multiply and cause damage to the new location, irrespective of their birth location.
Causes of Pulpitis
The innermost part of the tooth, the pulp, is protected with the enamel and dentine layers.
When pulpitis occurs, the layers get damaged, and the inflamed pulp reveals symptoms.
There are many causes why pulpitis occurs. Here are a few common causes of pulpitis:
- Dental decay and cavities
Our teeth are arranged in an arch. Cleaning teeth is necessary to prevent bacterial accumulation in caries-prone areas.
Over time, the plaque accumulates, and the bacteria feeds on the food particles left on the tooth. This, in turn, destroys the surface of the tooth, creating holes that lead to sensitivity or severe toothache.
- Trauma or injury to the tooth
Sometimes, a fall or a hit causes tooth fractures. The tooth fracture propagating from enamel, dentine, and root can directly affect the pulp, causing an inflammatory response within the pulp.
- Bacterial infection
Sometimes, gum infection can also cause irreversible pulpitis. The tooth is embedded in a bone surrounded by the gums.
When gums get infected, the bacteria get the opportunity to find their way to enter inside the tooth. The tooth becomes inflamed, causing pulpits.
- Untreated dental issues
Untreated dental cavities of a minor nature, like pits and fissure caries, can progress with time and reach the pulp.
Once the caries are extended, it will cause pain and discomfort, followed by irreversible pulpitis and pulp necrosis (pulpal death).
Types of Pulpitis
Pulpitis may be acute or chronic. Learning the types is essential to make the diagnosis of pulpitis. There are two types:
Reversible pulpitis
Such type of pulpitis is an acute inflammation of the pulp, which means it’s a short-standing inflammation of the pulp that usually happens when there is a small cavity or when your teeth have undergone attrition over some time.

Tooth fracture and cavity removal at a dentist can also lead to reversible pulpitis.
Symptoms
Usually, reversible pulpitis is symptomless; however, you may experience symptoms sometimes of a unique pattern.
Whenever you eat something cold, hot, or something sweet, you may experience sharp pain, which indicates reversible pulpitis.
The pain subsides with the removal of the stimulus. The normal pulp responds very differently to the stimulus provided.
On a normal pulp tissue, the pain initiates at a high temperature and continues to increase unless the temperature is released.
However, with the application of a cold stimulus, the pulpal tissue responds immediately, but the pain response diminishes with the increased intensity of the cold.
Diagnosis
Clinically, your dentist may look for prior pain and sensitivity history to rule out pulpitis from other tooth pathologies.
Further, he’ll look into your mouth for a cavity or a fracture before taking your periapical x-ray.
If needed, he may also perform an electric pulp test with an electric pulp tester.
On a periapical X-ray, a small translucency can highly denote the presence of a cavity and its proximity to the dental pulp.
Treatment
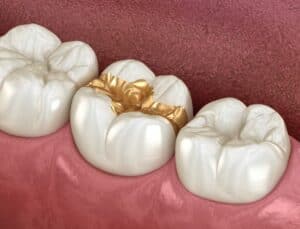
Pulpitis is reversible when the pulp returns to its normal state once the cause is removed. If a carious lesion appears on an X-ray, a dental filling can be done to treat pulpitis.
This will control the sensitivity of the pulp by insulating the pulp with a filling material.
In response to this, the pulp will deposit secondary or tertiary dentine to strengthen the pulp-filling barrier.
Irreversible pulpitis
Such type of pulpitis is the chronic inflammation of the pulp, which is more often a sequel to reversible pulpitis.
It’s a severe pulp inflammation where it will eventually die regardless of whether the cause of inflammation is removed.
Hence, the name is irreversible, which means the condition can never turn to normal no matter what.
The causes are similar to the cause of reversible pulpitis, but they are more intense. Like a large cavity in the mouth or a tooth fracture going down to the root.
Symptoms
Irreversible pulpitis may be symptomless and can appear with signs and symptoms.
With symptoms, you may suffer from spontaneous pain that will initiate without any stimulus like hot or cold.
The pain will usually start on its own and is poorly relieved by NSAIDs. The pain will continue for minutes and hours and is generally reported to increase with the change in position.
The pain can be episodic or continuous. The pain is usually sharp and dull and is not localized easily.
Diagnosis
Clinically, your dentist will ask a few questions about the symptoms you’ve experienced and the nature of the pain.
Moreover, he’ll perform an electric pulp test, heat test, and cold test before getting an X-ray done.
A hot stimulus on the tooth will result in an immediate painful response, while a cold stimulus will relieve the pain.
Treatment
A root canal treatment is the only possible treatment of pulpal inflammation in an irreversible state.
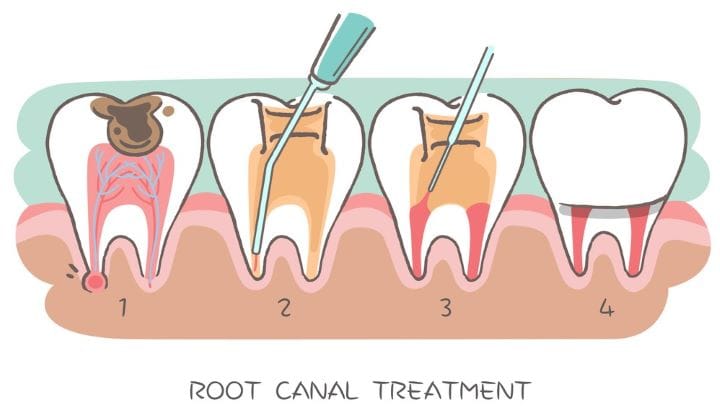
In worst-case scenarios, a tooth might need an extraction.
Symptoms of Pulpitis
- Toothache
The toothache due to pulpitis occurs spontaneously and is intense. The onset is sudden, followed by an extreme sensitivity to hot and sweet products.
The pain continues for hours and is poorly controlled by painkillers. The pain is throbbing in nature and can be defined as lingering.
The pain is poorly localized and can be felt radiating to the ears, head, and neck.
- Sensitivity to hot or cold temperatures
Whenever you’re suffering from pulpitis, you’ll see an improved threshold for pain against hot stimuli. With the increase in temperature, the pain increases. However, with ice cream or cakes, the pain due to pulpitis decreases.
- Pain while chewing
The affected tooth is painful when chewing because of the excessive pressure in the pulp chamber. This increases the pain on the affected side.
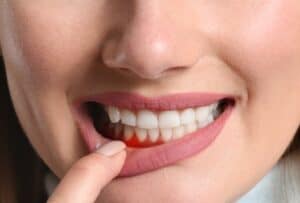
- Swelling in the affected area
The inflamed pulp with a lot of pulpal pressure can cause gum swelling around the affected tooth. The gum area would appear red and swollen. Sometimes, the swelling may appear due to bony inflammation around the affected tooth root, which is also called a periapical abscess.
Diagnosing Pulpitis
- Evaluation of symptoms
Whenever you reach the dental office with a complaint of pain, you’ll be asked a few questions to reach the diagnosis.
You’ll be questioned about the symptoms and the nature of the pain. Furthermore, you’ll be asked about the response of pain to hot and cold stimuli and the change in pain upon the change in position.
You’ll also be enquired about your medical and dental history before proceeding with a dental examination.
- Dental examination
Your dentist will visually examine your tooth for dental caries, cracks, and fractures. He’ll use a dental mirror and a probe for the aid before taking a dental X-ray of the affected tooth.
He may also perform an electric pulp test with an EPT device, a cold test, and a hot test for further confirmation.
- Xrays and imaging tests
Usually, a periapical X-ray or the bitewing X-ray of the affected tooth is taken to reach the final diagnosis. These will help analyze the internal structure of the tooth closely and look for cavities and cracks propagating within the tooth.
Complications of Untreated Pulpitis
- Periapical abscess formation
A periapical abscess is formed when the dead tissues inside the tooth accumulate at the apex of the root.
It’s a hub of bacteria that grows and lives in it. Removing the cause will treat the abscess. Sometimes, an incision and drainage is required to relieve the pressure.
- Spread of infection to surrounding tissues
The infectious sequelae of pulpitis are many. The untreated pulpitis can progress into periodontitis, cellulitis, osteomyelitis, sinusitis, meningitis, pericarditis, and even brain abscess. It means you shouldn’t take tooth inflammation lightly.
- Risk of tooth loss
Over time, the carious tooth undergoes massive decay. When the decay goes beyond the bone levels, the tooth remains no longer salvageable. It’s the stage when tooth extraction is a must.
Treating Pulpitis
- Medications for pain and inflammation
Dental pain can be treated with oral analgesics with a variety of medications. NSAIDs are effective at reducing pain.
According to the American Dental Association, NSAIDs act peripherally by reducing inflammation at the site where it’s occurring. Acetaminophen, aspirin, ibuprofen, and naproxen sodium are prescribed to patients.
Another class of drugs that are used to treat the pain of irreversible pulpitis is opioids, which include oxycodone, hydrocodone, and codeine.
These are often prescribed in combination with acetaminophen or aspirin.
- Pulpotomy
Partial removal of pulpal tissues in the cases where root formation is not completed is called pulpotomy.
It’s less invasive than root canal treatment and is usually performed in baby teeth and adults with incomplete tooth root formation.
This way, a decayed tooth is saved. In this procedure, the pulp is scooped out and removed from the crown portion of the tooth after anesthesing it.
- Root canal therapy
The sequel of the inflamed tooth can be lethal. Your dentist or endodontist will prescribe a root canal procedure to save a decayed tooth.
This procedure removes the inflamed or infected pulp from inside the tooth. The tooth is then cleaned and disinfected correctly.
It’s then sealed with a sealing material, followed by a dental filling and a dental crown.
- Tooth extraction as a last resort
If the tooth isn’t salvageable, no matter what, you’ll be prescribed dental extraction. It happens in cases where the tooth margin has decayed immensely and has gone below the bone levels.
Preventing Pulpitis
- Practicing good oral hygiene
As said before, one of the primary reasons causing pulpitis is dental caries. Without a genetic predisposition for dental caries, caries can only arise if oral hygiene is not maintained.

Proper brushing twice daily and flossing can reduce the chances of tooth decay tenfold. Dental hygiene maintenance is a pre-requisite when it comes to the prevention of decay.
- Regular dental checkups
Visiting the dentist twice annually is mandatory for your oral health. Sometimes, deep pits and fissures on your molars house bacteria in them, which causes caries.
Upon dental visit, you may identify those deep fits and issues and may get them filled with fissure sealants.
This is one preventive measure you can take only if you visit your dentist regularly.
- Prompt treatment of dental issues
Your negligence and delays in getting your dental appointments fixed can move a tooth from salvageable to a nonsalvegable one. For say, you had an irreversible pulpitis pain a year ago. The pain subsides within a few days, and you don’t see the dentist. The tooth that could have been saved with a root canal procedure a year ago now needs an extraction because you didn’t seek prompt dental care for your tooth.
Home Care for Pulpitis
- Using over-the-counter pain relievers
OTC painkillers are effective in managing acute to moderate pain. These work on peripheral receptors and mediators, causing them to shut off the pain pathway reaching the brain.
These are acceptable for relieving pain for a short period, but absolute pain release will only happen once the cause is removed.
- Avoiding extreme temperatures:
The irreversible pulpitis is exacerbated with hot foods and beverages and relieved with cold food. It’s better to avoid the intake of hot tea and coffee when experiencing symptoms of irreversible pulpitis.
- Rinsing with salt water:
Rinsing with lukewarm salt water rinses can help relieve the symptoms of irreversible pulpitis. Half a teaspoon of salt in 8 ounces of water is enough to relieve your symptoms.
Diet and Pulpitis
- Impact of diet on dental health:
You need to be very particular about selecting good food for your overall health and the health of your gums and teeth.
Sticky foods like candies and chips are very fond of promoting tooth decay and gum diseases. The plaque forms a thin, invisible, sticky covering on all of your teeth.
The plaque is a biofilm of multiple bacteria covering the tooth surface. Whenever you eat sugars, the bacteria produce acid that can attack the tooth, which leads to tooth decay.

So, it’s necessary to select the healthy food for your overall health carefully
- Foods to avoid for individuals with pulpitis
Stay away from certain food types like sticky candies and sweets. Avoid lollipops, caramel candies, and sweets, as they are great at producing massive amounts of acids to destroy your teeth.
Other food products to avoid are potato chips, soft breads, carbonated soft drinks, and alcoholated products.
- Foods that promote dental health
Eat foods that are rich in fiber. These foods act as natural cavity defenders and improve the overall salivary flow in the oral cavity.
These also restore the mineral content of your cavity.
A few food items that are good for your oral health are cheese, yogurt, milk, green and black teas, and fluoridated water.
Pulpitis in Children
- Unique considerations for pediatric pulpitis
Pulpitis in baby teeth is common and is presented with a sharp, aching pain in the tooth.
The inflammation of the pulp in the baby tooth is similar to an adult tooth, but the rate of progression is quicker in the baby tooth than in the adult tooth.
The primary cause of pulpitis in pediatric patients is the dental caries. Milk teeth are less dense and have thinner enamel and dentine.
It means the caries can reach the pulp 2x faster in milk teeth when compared to adult teeth.
- Treatment options for children
Pulpitis in children can be treated in two ways:
1) Pulpotomy (partial removal of pulp tissue)
In this procedure, the pediatrician will anesthetize the tooth and remove the caries from the diseased tooth.
He will carefully remove the infected pulp tissue and place a special material called MTA to save the remaining pulpal tissue.
He will later fill the tooth with filling material or may prescribe a stainless steel crown on top of it.
2) Pulpectomy (Complete removal of pulp tissue)
To save the tooth from extraction, the pediatrician will completely debride the pulp canals and fill the canals with a sealing material.
This is s conventional root canal procedure for the baby teeth. If needed, a tooth filling will be done later, followed by a stainless steel crown.
3) Extraction
Sometimes, extraction will be prescribed to get rid of the pain in the tooth.
Prevention of Pulpitis In Children
The best way to prevent pulpitis in children is to teach them to maintain oral hygiene and get their teeth checked with a dentist every 3 to 6 months.
It’s even advisable to improve their overall eating habits and to teach them to eat foods rich in fiber and minerals.
FAQs
Why does irreversible pulpitis follow with a severe toothache?
The pulpal tissue is enclosed in a closed chamber. When the pulp inflames, the pressure within the chamber increases.
The inflammation improves the blood supply and causes the release of pain-causing substances and pro-inflammatory substances.
The increased pressure will cause the vessels within the chamber to strangle, subsequently leading to pulpal necrosis.
The nerve fibers within the pulp are responsible for giving you a painful sensation of dull and continuous nature.